Jill J. Easton | Originally published in GameKeepers: Farming for Wildlife Magazine. To subscribe, click here.

Ticks are a fact of life for anyone who spends time outdoors. A tick attack can be as surreptitious as the dozens of small dots that are seed ticks digging into an ankle, or a larger stealth “attacher” like a dog tick, lone star tick or blacklegged tick, that digs-in and hides in those moist hidden places like an armpits, groins or navels.
Animals, especially birds and mammals under stress, can also be severely impacted by ticks. Deer, elk, turkeys, bears,raccoons, bobcats, coyotes and even rabbits can get ticks. In years when mast crops fail or weather is extremely harsh, ticks can further weaken wild animals to the point that they are unable to fend off other diseases.
No matter where they begin chewing their way to blood, tick bites can cause weeks of itching, scratching and annoyance. Unfortunately, these small arachnids (that’s right, they’re members of the spider family) are also carriers of dozens of life-threatening illnesses that they pick up as they suck blood during three of the four stages of their lives.
Lifestyles of ticks
A tick begins life as an egg left on the ground in a damp protected area. Ticks require moisture for each stage of their metamorphosis, so they generally don’t thrive in extremely dry country. Most tick species require three to seven blood meals before becoming adults.
Ticks get blood by cutting a hole in the host's epidermis; inserting the hypostome (head and mouth parts) completely into the skin and then excreting an anticoagulant which keeps the blood from clotting. Since ticks breathe through respiratory plates on their bodies, they can totally immerse their heads into the host’s skin.
Larval ticks generally attach to birds or small mammals to score first blood. When they are full, the tiny ticks pull out, let go and drop back to the ground where they eventually change into nymphs.
The nymphs wait hanging on to grass blades, leaves or branches until they can latch on to another warm-blooded host. Unlucky nymphs can wait months or even years, until they harvest their second meal. After feeding, a process that takes several days, the nymphal ticks again drop back to ground level to molt and eventually become adults.
Shield Yourself from Ticks
Preventing ticks
- Wear high boots or tuck your pant legs into your socks and spray all outer clothing with DEET or permethrin. Pay special attention to cuffs, collars, caps or wherever ticks have access to your body.
- Insect Shield clothing repels ticks and mosquitoes. The Insect Shield process binds a proprietary permethrin formula to fabric fibers—resulting in effective, odorless insect protection that should last the lifetime of the apparel.
- Certain permethrin sprays may also be sprayed in gardens or areas around your home to kill and/or repel the nasty little creatures.
Removing ticks
- Quick tick removal is important. If the tick isn’t deeply imbedded scrape it off with a flat hard surface like a credit card.
- If the tick is imbedded, grasp the head with a pair of tweezers as close to the skin as possible and pull straight up. Don’t squeeze the tick’s body. That will force more bacteria into the bite area. Make sure you get the head.
- For seed ticks, put a piece of duct tape over the tick(s), press down and then pull the duct tape off. Consider the tweezers method in areas with lots of hair.
Controlling ticks
- Ticks desiccate quickly and must stay close to moisture. A gravel walkway will provide a barrier that is difficult for ticks to cross. Small areas inside the gravel barrier can be sprayed to kill ticks. There are a number of products that kill the animals.
- White-footed mice should be eradicated if seen. These rodents are believed to be the primary contact where larval ticks pick up the bacteria that lead to diseases.
- Guinea fowl-are great at controlling bugs, especially ticks around houses and outbuildings. Chickens also do this to a lesser degree.
- Adult ticks go through the same luck-of-the-leg victim catch, called questing, as the other stages. Or they may chase their food as seeker ticks that actually go on the attack, tracking nearby emissions of carbon dioxide. Any- one who’s ever had a rogue tick under several layers of hunting clothes knows how fast they can move.
- Mature male ticks are much less likely to bite than their female counterparts. Males often wander around on the host animal looking for females to mate. When they are again full the females drop-off onto the ground and lay the thousands of eggs that begin the cycle again.
Tick-borne diseases
Lyme disease, anaplasmois, Colorado tick fever, ehrlichiosis, Q fever, Southern tick associated rash illness (STARI), powassan encephalitis and tularemia are some of the diseases that can be caught from tick bites.
Ticks pick up bacteria that carry the diseases they spread from a wide variety of hosts, but rodents are the major culprits. Ticks and the diseases they spread are found around the world and almost everywhere in North and South America.

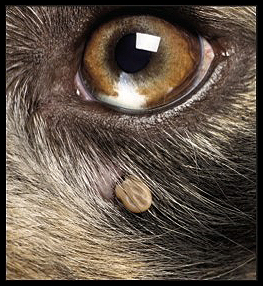
the spider family are also carriers of
dozens of life-threatening illnesses
that they pick up as they suck blood
during three of the four stages of their
lives. The bite in this photo transmitted
lyme disease to the unfortunate
recipient.
In our little town of Calico Rock, Arkansas, population 1,543 - in less than three days of asking I found several dozen people who had “tick fever,” three who tested positive for the antibodies for Lyme disease and two who had tick-borne meat allergy.
Tick fever
Probably the most commonly diagnosed tick fever is ehrlichiosis, caused by bacteria in the saliva of American dog ticks. There are two kinds of tick fever: Rocky Mountain and Colorado. Rocky Mountain tick fever can be fatal if untreated. The infection is passed to humans or dogs by the tick’s saliva during the bite. In any group of outdoors folks there will probably be a number who have had this disease, but it isn’t limited to people who spend time outdoors.
“Last summer was extra hot, so we let the dogs stay inside during the day and they brought in ticks,” explained John Yutsus, who runs a coffee shop and bakery in Calico Rock, Arkansas. “I found a tick dug in close to my hip bone. I figured the dogs brought it in. I pulled it off and didn’t think about it again.”
Several days later John discovered a rash across his lower stomach. “For a few days I thought it was some kind of heat rash since the temperatures outside were well above 100 degrees every day,” Yutsus said. “Then I started feeling cruddy; dull and dragged-out, it was almost like a case of the flu. After a few more days my wife made me go to the doctor. When I described the symptoms, Dr. Knight immediately diagnosed it as tick fever and put me on doxycycline. Within a few days I was fine.”
Like most tick transmitted diseases, "tick fever" is usually diagnosed by the symptoms. The antibiotic doxycycline is the preferred treatment for any tick-borne disease. People who are not able to take doxycycline are usually given chloramphenicol, or ciprofloxacin.
Lyme disease and Rickettsia
your pets and if the ticks do not attach
to your pet, your pet can carry the ticks
into your household. It’s important to
use repellents and check your pets
often.
“Lyme seems to be a “badge of honor” for some ... it's also hard to diagnose, or definitively test, and it is very serious if untreated,” said Doctor Allan Houston, a Professor of Forestry, Wildlife and Fisheries at University of Tennessee. “Many folks who have had a significant number of tick bites have been exposed to some form of rickettsia and some of the types mimic lyme. Many of these folks have been treated for lyme and the effective treatment for lyme is the same as for rickettsia and the patient becomes well. They are convinced they had lyme and they will punch you in the nose if you suggest it might not have been lyme.”
True "lyme disease" can only be proven by a blood test that looks for antibodies for the disease, and like tick fever the treatment is much cheaper than the test. People generally catch lyme after a deer or black legged tick has remained imbedded in their skin for a minimum of 36 hours. This gives the bacteria time to cross over from the tick into its human host.
“A bulls eye appeared on the left cheek of my butt a few days after I’d pulled off a dark brown tick,” said Jim Spencer, a turkey hunter and trapper who spends a lot of time outdoors, also from Calico Rock. “Then I started having chills and fever along with swollen lymph glands and a near constant headache. I knew this could be a tick disease so I got antibiotics from my doctor, who assured me there was no lyme disease in Arkansas. It wasn’t until years later when I had a blood test during a physical that it was confirmed that at some time in the past I had lyme.”
Spencer was one of the lucky ones. If lyme disease goes untreated it can eventually cause nervous system abnormalities, such as numbness, pain, irregular heart rhythm, partial paralysis of facial muscles, and meningitis.
Since rickettsia has similar symptoms to lyme, the diseases are often confused. Many people exposed to rickettsia feel bad for a few days then their immune system fights it off, leaving them with the impression that they simply had a bug of some sort. They did.
“They often find out much later when they test positive for “previous exposure” to rickettsia,” explained Dr. Houston. “Many folks who have had a significant number of tick bites have been exposed to some form of rickettsia.” There are a number of rickettsia species. Some of the diseases do not even have common names.
Meat allergies

nice batch of squirrels. In
preparation for this article she
questioned people in her
community of Calico Rock,
Arkansas, and had no problem
finding numerous people that had
been affected by tick carried
diseases.
Lone star ticks, readily identifiable by the white dot or “star” on their backs, have been getting a lot of bad press lately. The reason should put fear into every carnivorous human. A bite from a lone star tick can give humans an untreatable allergy to red meat. It’s bad enough that they can transmit ehrlichiosis, but even worse, their saliva can carry an antibody that causes the immune system to overreact to sugars found in red meat. This causes an allergic reaction that usually shows up as itchy, burning hives all over your trunk and back.
Tom Hearn retired to the Ozarks, planted a big garden and spent most of his time outside working on building projects around his house. Since his land backed up to a wild area, it wasn’t unusual for him to find and remove several ticks each evening when he cleaned up.
“One night my back started itching while I was watching television after dinner,” said Hearn. “I went into the bathroom and looked in the mirror at my back and saw a rash. About an hour later spots showed up all around my body. Then the palms of my hand started itching. My hands had water filled pustules like a bad sunburn, all over. Shortly, I started to have trouble breathing. I knew it was time to get to the emergency room.”
The doctor treated him with an injection of allergy medication. Within hours all the symptoms were gone. He went to an allergist and got the standard scratch tests done, but nothing caused a reaction.
Hearn kept a log of everything he ate, plants he touched and anything that seemed to bring on problems. After several weeks of eating very carefully Hearn and his wife ate hamburgers at a local restaurant and the rash showed up again.
“Every time I ate red meat the rash returned,” Hearn said. “Chicken, fish and dairy products didn’t bother me. It’s something that just happens with red meat.” Unfortunately, he isn’t the only person around Calico Rock who has this meat allergy. The problem was that no one made the tick/meat connection until recently.
"Meat allergies are not very common," says Thomas Platts- Mills, MD, professor of medicine and head of the division of Allergy and Clinical Immunology at the University of Virginia Medical Center, who first identified that the meat allergy came from a tick bite. “This is truly the first example we've found of a food allergy being cause by a bug bite."
We must research ticks and the diseases they carry. A new study may find ways of controlling marauding ticks. Ames Plantation in southwest Tennessee is the 18,400 acre home of the National Field Trial Championship for All-Age Bird Dogs and a place where quail and deer are intensively managed. It is also one of the few places where ticks are under intensive study.
Complaints from co-workers, sportsmen and his own experience led Dr. Allan Houston to notice a huge increase in tick numbers in the central part of the country. Dr. Houston was in a unique position to do something about the situation. He is not only Director of Forest and Wildlife Research and Management at Ames, but is also a professor of Forestry, Wildlife and Fisheries at the University of Tennessee.
“It was apparent tick populations were on the increase locally and across the mid-south,” explained Dr. Houston. “I became interested in the population trends and also in what I suspected were a suite of diseases that were over-diagnosed,” Dr. Houston said. “Nearly everyone I knew had been treated for lyme. Perhaps something else was mimicking it, or doctors were being overly cautious, or patients were being overly strident.”
“Last summer, students collected ticks on Ames,” Houston said. “Several things were of particular interest and a couple of things were surprising. None of it was particularly pleasing.” Ticks were collected by dragging a cloth across the ground on specific sites and along preset routes. After dragging for 30 seconds the cloth was inspected and ticks collected. Questing ticks were caught this way. The second collection method was to leave a cloth out overnight with dry ice in the center to mimic a CO2 emitting critter. Seeker ticks were caught in this carbon dioxide trap.
More than 12,000 ticks were collected, unfortunately, there were plenty left for the future. “The study examined different habitats and assessed the risk in each,” Dr. Houston continued. “Are you more or less likely to pick up a passenger in grassland habitats, pine, hard- woods? The results are not complete, but I have no doubt that a large percentage of the ticks carry bacteria dangerous to humans.” “In our part of the world, the lone star tick is a big player, they account for much of the torment that we have endured,” said Dr. Houston. “It is a species that has invaded and prospered. The lone star is aggressive and does not mess around; it finds a place to bite and it bites.” Lone star populations have exploded for any number of reasons, but likely the species expanded as the weather became warmer.
Suspect a tick bite-get treated
It doesn’t really matter what kind of tick chews its way into your skin and blood. If you start feeling bad after finding one of the tiny eight-legged monsters imbedded in your skin, don’t wait. Go see a doctor.
The bottom line, as Dr. Houston puts it is simple and smart, “Tick bite(s) plus fever and malaise equals doxycycline.”